Diabetic retinopathy is a complication of small blood vessels and is characteristic of both type 1 and type 2 diabetes. The prevalence of diabetic retinopathy is related to the period of developing diabetes. After about 20 years of developing diabetes, we find that almost all people with type 1 diabetes, and about 60% of people with type 2 diabetes, have had diabetic retinopathy to some degree.
And with the question of Dr. Muhammad Hantira, Assistant Professor, Honorary Professor, Ophthalmology Department, Umm Al-Qura University, Saudi Arabia
Explain to us that diabetic retinopathy is dangerous for the ability to see. About 86% of blindness cases among patients with type 1 diabetes can be linked to diabetic retinopathy, while the percentage among people with type 2 diabetes, among whom other eye diseases are prevalent, is close to approximately one third. In general, diabetic retinopathy is the most common cause of new blindness in the 24-47 age group.
Dr. Hantira explained:
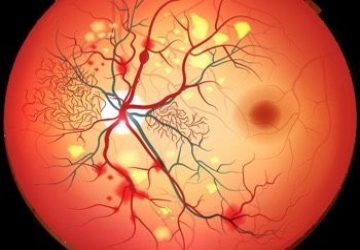
The onset of diabetic retinopathy may be accompanied by advanced blockage of blood vessels, and then penetration of the walls of blood vessels to their surroundings, followed by the growth of cells and the emergence of new blood vessels, in the retina and on the posterior surface of the vitreous.
Dr. Hantereh noted:
Until vision loss caused by diabetic retinopathy, it is the product of a combination of systems. Central vision disturbances may be caused by macular edema in the yellow area on the retina, and new blood vessels can bleed and add other complications to the vitreous, or even crack and detachment of the retina.
Treatment of diabetic retinopathy
Dr. Hantira explained:
That there are treatment methods that can prevent or hinder the occurrence of retinopathy in diabetics as well as prevent vision loss in a large number of diabetic patients.
Intensive diabetes treatment, aimed at achieving a good level of control over blood sugar levels, may prevent or hinder the progression and development of diabetic retinopathy. Also, treatment of early photocoagulation by laser can prevent vision loss in a large number of patients.
Dr. Hantereh noted:
In some cases, those who suffer from diseases that pose a threat to their sense of vision may not show any symptoms, and therefore it is extremely important to undergo periodic examinations, in order to diagnose retinopathy if it occurs. The base of the eye imaging is one of the tests that have a higher probability of detecting retinopathy than the regular tests. This, despite the fact that the regular tests are better, in order to detect the enlargement of the retina associated with molecular tumors, and it is possible to diagnose the growth of new and minute blood vessels in the area of the optic nerve head, or in other places on the retina.
Dr. Hantereh's advice for follow-up medical evaluation for diabetic patients:
• It is recommended that patients who have had type 1 diabetes undergo a comprehensive eye examination, with dilated pupils, at an ophthalmologist or optometrist, after 3 to 5 years have passed from the onset of diabetes. Likewise, patients who have had type 2 diabetes must undergo a comprehensive initial eye examination, at an ophthalmologist or an optometrist, shortly after they have been diagnosed with the disease.
• Patients with type 1 and type 2 diabetes should return to have an eye examination every year, at an ophthalmologist or optometrist, provided that he has knowledge and experience in diagnosing diabetic retinopathy. If the condition is advanced, the interval between examination and the other should be shorter.
• Women with diabetes who wish to become pregnant and give birth should undergo a comprehensive eye examination and receive counseling about the risks of developing or exacerbating diabetic retinopathy. Likewise, pregnant women with diabetes must undergo a comprehensive eye examination during the first trimester of pregnancy, and continue to monitor and follow up their condition throughout the months of pregnancy.
• Patients who have had diabetic retinopathy of any degree require immediate treatment by an ophthalmologist with experience and knowledge in the field of diabetic retinopathy. Treatment of diabetic retinopathy with a laser, at this point, would help reduce the risk of severe vision loss by 50%.
• Patients who have lost vision due to diabetes need vision restoration and treatment, with the help of an ophthalmologist or optometrist, provided that they are with appropriate rehabilitation and experience in the field of vision impairment.
With us, you are in safe hands, and we wish you a speedy recovery